Common Pelvic Floor Dysfunctions and Diagnoses
Listed below are some of the most commonly diagnosed dysfunctions of the pelvic floor. Some symptoms of these disorders are more troublesome than others however, no matter how mild or severe your symptoms are, there is no better time than now to seek treatment to start improving your quality of life! Leak when you jump? Read on! Feelings of vaginal pressure or heaviness? Read on! Hip, low back or pelvic pain? Read on! Diastasis recti concerns? Read on!
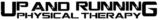
Urinary Incontinence
Urinary incontinence is the involuntary loss or urine, or accidental peeing, during certain activities. There are several different causes and types of urinary incontinence ranging from leaking caused by jumping activities all the way to not being able to physically get oneself to the restroom on time. Here are some of the most common types: Stress incontinence is leaking due to increased intra-abdominal pressure that places downward pressure onto the bladder which can result in leaking when we have a pelvic floor dysfunction. Common activities of daily living that increase our intra-abdominal pressure and may cause this type of leaking include laughing, sneezing, coughing, jumping or even heavy lifting. Another common type of incontinence is urge incontinence where we may feel an intense and sudden urge to urinate followed by the sudden involuntary loss of urine.
This is also sometimes referred to a “latchkey or lock-and-key” incontinence – where, for example, you’ve just finished a long day of work; you’ve driven home and as you are putting your key in the door you feel a sudden intense urge to pee, and you are unable to make it to the bathroom in time. Overflow incontinence is the inability to fully empty the bladder therefore leading to frequent, small amounts of leakage. Functional incontinence refers to incontinence that occurs because a person has a physical or mental impairment that prevents them from getting to the bathroom in time after feeling the urge, or not feeling or understanding the urge signals. And finally, mixed incontinence is a combination of any of the types of incontinence mentioned previously, with the most typical combination presenting as stress and urge incontinence.
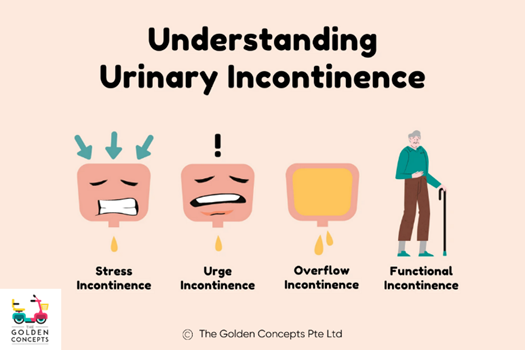
Pelvic Organ Prolapse
Decreased support of our pelvic organs, from the pelvic floor, may lead to descent or drooping of one or multiple of the pelvic organs into or outside of the vaginal canal and anus. This decreased support and increased downward pressure on the pelvic floor may be due to, or cause increased risk; pregnancy, labor and delivery, obesity, COPD or chronic respiratory disorders and connective tissue disorders. The following are the various types of prolapse – cystocele (prolapse of the bladder), urethrocele (prolapse of the urethra), uterine prolapse (prolapse of the uterus), vaginal vault prolapse (prolapse of the vagina), enterocele (small bowel prolapse) and rectocele (prolapse of the rectum).
Depending on the type of prolapse, symptoms may vary, but generally people report feelings of pressure or heaviness in the abdomen or pelvic region, pain with intercourse, leaking, low back pain or the need to insert a finger intra-vaginally or intra-rectally to urinate or defecate. Prolapse is graded on a scale of 0-4, with 0 being no signs of prolapse and 4 being the highest severity of tissue descent. However, it is important to note that the degree of prolapse does not dictate your symptoms. You may have a very mild prolapse but have symptoms that bug you on a daily basis or you may have a more severe prolapse, but symptoms are less noticeable.
Pelvic Girdle, Hip and Low Back Pain
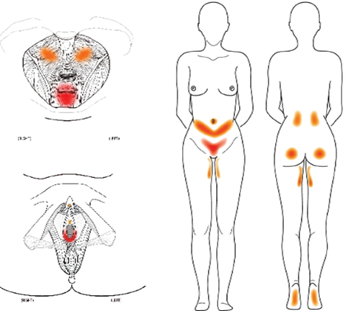
The pelvic floor muscles attach from the lowest part of our spine (the coccyx or tailbone) and attach to the front of the pelvic bowl and have a very close relationship with some of our hip muscles too. Therefore, the strength and mobility of our lower back and hips play a crucial role in optimal functioning of the pelvic floor. Dysfunction of one of these areas may lead to dysfunction in another area as the body tries to compensate and pick up the slack. There is evidence that shows that people with low back pain may have decreased function of the pelvic floor muscles compared to those who do not have low back pain.
Additionally, we may have a body part that is “referring” pain to the pelvic floor and so our symptoms may present in the pelvic floor, but the origin of the dysfunction is elsewhere, with the most common referral pattern being the adductors referring pain to the pelvic floor. The pelvic floor muscles themselves may also refer pain to the low back, hip or even the abdomen. Another cause of pain may be the resting state of the pelvic floor muscles. Pelvic pain, especially during intercourse, may be due to pelvic floor muscles that are over-recruited (their resting state is too tense) and struggle to relax during intercourse which may lead to pain, or even then inability to become aroused or reach climax.
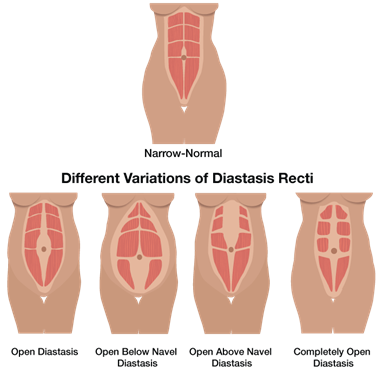
Diastasis Recti Abdominis (DRA)
Thinning of the linea alba which is the fascia or connective tissue between our sets of “6-pack ab” muscles (the rectus abdominis) is termed diastasis recti abdominis (DRA). This phenomenon is most commonly thought of in the postpartum period but can happen to any person, at any stage of life; infants can have a DRA and it is common in men too. By the end of the third trimester, all women will have some degree of ab separation as the linea alba thins and spreads prior to delivering their baby and this is 100% normal and necessary to accommodate for the growing uterus and fetus. We generally see closing of this gap by around 8 weeks postpartum.
Elasticity of the tissue may have been lost due to this stretching and the gap may not close between the left and right side of the superficial abdominal muscles because of this. Around 40% of women will have a diastasis up to 6 months postpartum. Although DRA is not a pelvic floor dysfunction, it is a pressure management issue (similar to stress urinary incontinence). When we are unable to maintain our intra-abdominal pressure during activities, it may present itself as a doming or coning of the central area of the abdomen when contracting the abs or doing a core exercise.
This loss of tissue elasticity between these muscles may make it feel like your core is weak and it may make doing certain activities slightly more challenging, but having this separation is not a painful experience. If you look on the internet “how to fix DRA” you will find lots of lists of exercises that you should and should not be doing. This is an outdated outlook on conservative management of this condition. There are no magic exercises that will cure diastasis and there are no specific exercises that should be avoided all together. You should monitor your symptoms during an activity or exercise and progress or regress based on your ability to manage that pressure and whether or not you are excessively bulging, coning or doming. We want to load the tissue to improve its strength and it’s important to incorporate a progressive overload approach to this condition just as we would any other “weak” muscle!
If you want to know the best ways to treat these “dysfunction and diagnoses,” manage symptoms and improve your quality of life using an evidence-based and individualized approach, give us a call at 970-480-7705.
 Dr. Sam Greig.
Dr. Sam Greig.
This blog was written by our very own
Pelvic/Women’s Specialist, Dr. Sam Greig.
References:
Arab AM, Behbahani RB, Lorestani L, Azari A. Assessment of pelvic floor muscle function in women with and without low back pain using transabdominal ultrasound. Manual therapy. 2010 Jun 1;15(3):235-9.