As a healthcare professional, I recently had a patient named Anna* who came to me for a pelvic floor evaluation. Anna is a 50-year-old woman who has two grown adult children and recently retired. She loves to hike and run and was enjoying her newfound freedom until she began experiencing bothersome pelvic floor symptoms that she had never felt before.
Despite having two vaginal deliveries around 20 years earlier, Anna thought she was in the clear for leaking and had never experienced any incontinence. She was also enjoying an increased libido now that she did not have children in the house. However, she noticed that sex seemed to be more and more painful. After experiencing these symptoms and feeling frustrated, Anna consulted with her primary care physician, who concluded that she was likely in perimenopause.
In this blog, we’ll delve into the world of pelvic floor evaluation and how it can help women like Anna understand and manage their symptoms. We’ll explore common symptoms and conditions that affect the pelvic floor, such as incontinence, painful sex, and perimenopause, and provide insights into the treatment options available to manage them.
From pelvic floor exercises and physical therapy to medications and surgery, we’ll cover everything you need to know about pelvic floor evaluation and treatment. Whether you’re experiencing pelvic floor symptoms for the first time or have been struggling with them for years, this blog will provide you with valuable information and resources to help you manage your symptoms and improve your quality of life. So if you’re ready to take control of your pelvic floor health, keep reading to learn more about pelvic floor evaluation and treatment.

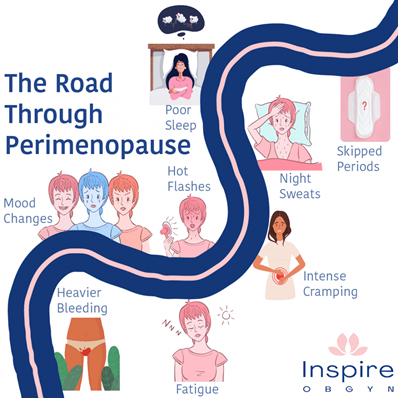
Perimenopause, or the menopausal transition, is the time leading up to menopause which often begins in the mid-40s, and is associated with lots of bothersome symptoms such as hot flashes and mood swings. Menopause is defined as 12 months after the last period, and the average age of menopause in the US is 51 years old. It can be difficult to know if you are in menopause and not just experiencing irregular periods in the perimenopausal phase. The postmenopausal period is any time after menopause.
Menopause is NOT a disease or a disorder and is a natural biological process. However, the changes that occur are very real and can be extremely frustrating, especially because (as usual) menopause is hardly discussed as a society, symptoms are often “normalized” and people do not know that treatment and help even exist!

During menopause estrogen levels begin to decrease which may lead to the following common signs and symptoms:
- Changes in periods
- Hot flushes (flashes)
- Incontinence and leaking
- Insomnia and trouble sleeping
- Vaginal dryness
- Pain with intercourse
- Changes in mood
- Weight gain
- Joint and muscle aches and pains
Several of these symptoms are grouped together and termed “genitourinary syndrome of menopause” (aka GSM) which include what Anna was experiencing: painful sex, vaginal dryness and decreased lubrication, urinary frequency and urgency, urinary leaking, post-coital bleeding, recurrent UTIs and prolapse. GSM is a very commonly underdiagnosed condition despite 50-70% of the postmenopausal population reporting at least one symptom of GSM, and up to 70% of postmenopausal women displaying pelvic floor dysfunction. Although the menopause phase is most typically associated with hot flashes, GSM symptoms have a higher negative impact on quality of life and unfortunately do not typically spontaneously resolve and can get worse if left untreated.
If you’ve read any of my other blogs, you know that PT can help with several of the symptoms listed above! Pelvic floor physical therapy has great success rates treating urinary urgency and frequency, pain with intercourse, as well as addressing leaking.

PT cannot help improve or decrease vaginal dryness however ensuring you are using enough lubrication (preferably water-based) can be extremely helpful to minimize pain and post-coital bleeding caused by increased friction. A vaginal moisturizer can help to decrease the uncomfortable sensation of a dry vulva.
A pelvic floor physical therapist can also help devise a strengthening and cardiovascular program. Both are essential components of successful aging and minimizing the negative effects of changing hormones. These hormonal changes make weight gain easier, bones more brittle, and building muscle mass harder. It is imperative to continue to strength train to sustain and build your muscle mass as well as improve bone density. Strength training does not have to be intimidating, and gym selfies are not required but think about all of the activities that we do on a daily basis that require leg and arm strength – getting up and down from a chair or off of the floor, climbing stairs, carrying groceries and holding grandchildren.
Cardiovascular exercise is also extremely important due to the increased risk of cardiovascular disease women experience (and not to get too morbid here, just trying to shock you into action – heart disease is the leading cause of death in US women). Both cardiovascular exercise, strength training, and a good diet can help manage weight gain.
Anna’s decision to take a combined approach of pharmacological and conservative treatments to manage her pelvic floor symptoms proved successful. She was delighted to report that she is once again enjoying intimacy with her partner.
At our practice, we believe in being a part of your team and guiding you through the menopause journey, ensuring that you feel empowered and equipped to deal with significant life changes. Our team of healthcare professionals understands that managing menopause can be a challenging experience. With our expert guidance, we can help you navigate through the various options available to you.
Whether you opt for pharmacological treatments, conservative methods, or a combination of both, our team will work with you to develop a personalized treatment plan that is tailored to your specific needs.
We believe in educating our patients about the different treatment options available to them and providing them with the necessary resources to make informed decisions about their health. With our guidance, you can feel confident in managing your menopausal symptoms and regaining control of your life.
So if you’re struggling with menopausal symptoms and are looking for a supportive team to guide you through the process, look no further. Contact us today and take the first step towards feeling empowered and equipped to deal with significant life changes.
* Anna: name changed for patient confidentiality

This blog was written by our very own Pelvic/Women’s Specialist, Dr. Sam Greig.
* * *
References
https://www.nia.nih.gov/health/what-menopause#:~:text=Menopause%20is%20a%20point%20in,between%20ages%2045%20and%2055.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7212735/
https://www.mayoclinic.org/diseases-conditions/menopause/symptoms-causes/syc-20353397
https://www.cdc.gov/heartdisease/women.htm
https://pelvicpainrehab.com/menopause/19572/solutions-for-menopausal-women-with-gsm-and-pelvic-floor-dysfunction/
* * *
Thanks for reading! If you’d like to learn more about who we are and what we do, click this link: https://upandrunningpt.com/