Did your doctor tell you to perform Kegels after giving birth and then give you the go ahead to resume normal activity at 6 weeks post-partum? Were you told by a friend that doing Kegels would “tighten up down there?” Well, I’m here
to set the record straight on who should, and maybe more importantly, who should not be doing Kegels.
Define Kegel
First, let’s start with the basics and define what a “Kegel” is. A Kegel is a pelvic floor muscle contraction (named after Arnold Henry Kegel, an American gynecologist) that is performed to strengthen the pelvic floor (PF). The term
has become somewhat mainstream with is connotations to sexual function, the selling of vaginal weights and mention in popular TV shows such as Sex and the City.
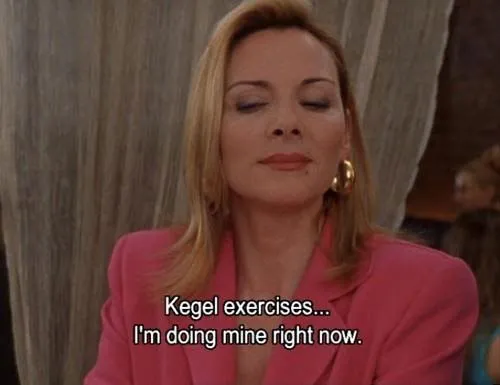
So where is the pelvic floor located and what does it do? The pelvic floor is made up of three layers of muscles that lie between the pubic bone in the front of the pelvis and your tail bone at the bottom of the spine. These muscles
are all skeletal muscles which means that they are under our voluntary control and can be strengthened and lengthened (just like the biceps or quads!).
The pelvic floor has many functions which include maintaining continence, bowel and bladder emptying, sexual functions as well as providing support to the pelvic organs, spine and pelvic girdle1. Dysfunction with the
pelvic floor can lead to pelvic organ prolapse, defecation and voiding problems, leakage, sexual dysfunction and pelvic pain. PF dysfunction may be due to a weak PF, a tight PF, incoordination of the muscles of the PF or several
other reasons.
Kegels can play an important role in the treatment of urinary incontinence and pelvic organ prolapse in the case of weak PF muscles to strengthen the pelvic floor to prevent leakage and provide support for the pelvic organs.
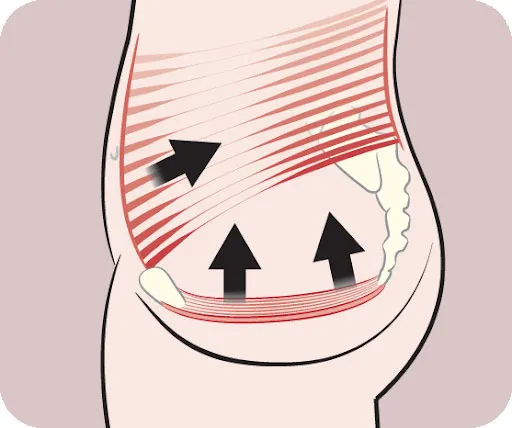
However, just as a person can have a weak pelvic floor that needs to be strengthened, a person can also have a hypertonic, or tight, PF that needs to be retrained to relax and lengthen. This is called “non-relaxing pelvic
floor dysfunction.” If you’re having trouble understanding this concept, think of the biceps. If they are weak you would want to strengthen them by doing a shortening contraction such as a bicep curl. However, if they are short and
contracted and you are having trouble straightening your elbow you would want to lengthen the muscle to regain the full range of motion of your elbow. The same concept applies to the PF.
When one tries to strengthen a muscle that is already in a hypertonic, shortened state, it can lead to further hypertonicity which may in turn exacerbate symptoms. This makes it counterintuitive to strengthen a muscle that is unable
to fully relax or move through its full range of motion or begin a concentric contraction from a normal resting length2. Just because a muscle is “tight” does not mean that the muscle is “strong.” A tight muscle has
a suboptimal length-tension relationship which reduces its force generating capabilities.
Additionally, you may have a hypertonic PF with underlying weakness which makes getting the correct diagnosis so important as this will guide treatment.
Kegels can also be a challenging exercise to perform correctly because the result of the contraction is not easily seen (compared to a bicep contraction in which you can see your elbow bend). Oftentimes people perform them
incorrectly by straining and bearing down instead of squeezing and lifting up which can also exacerbate symptoms when performed repetitively.
Not everyone should be doing Kegels at every stop light. Even those prescribed with Kegels will be given a specific number to do each day with variations in sets and for how long to hold each contraction. Every human is different
and therefore every treatment approach will be different.
If you want to know how you can manage your pelvic floor symptoms, schedule an appointment with our trained pelvic health physical therapist. They MAY or MAY NOT assign you Kegels based on your individual presentation. There is no
“one size fits all,” standardized approach for managing pelvic dysfunction.
Bottom line: not everyone should be doing Kegels. Strengthening without a formal assessment first may be doing more harm than good.

This blog was written by our very own Pelvic/Women’s Specialist, Dr. Sam Greig.
References
- Faubion SS, Shuster LT, Bharucha AE. Recognition and management of nonrelaxing pelvic floor dysfunction. Mayo Clin Proc. 2012;87(2):187-193.
- Prendergast S, Weiss. Screening for Musculoskeletal Causes of Pelvic Pain, Clinical Obstetrics and Gynecology: December 2003 – Volume 46 – Issue 4 – p 773-782