Understanding and Managing Constipation
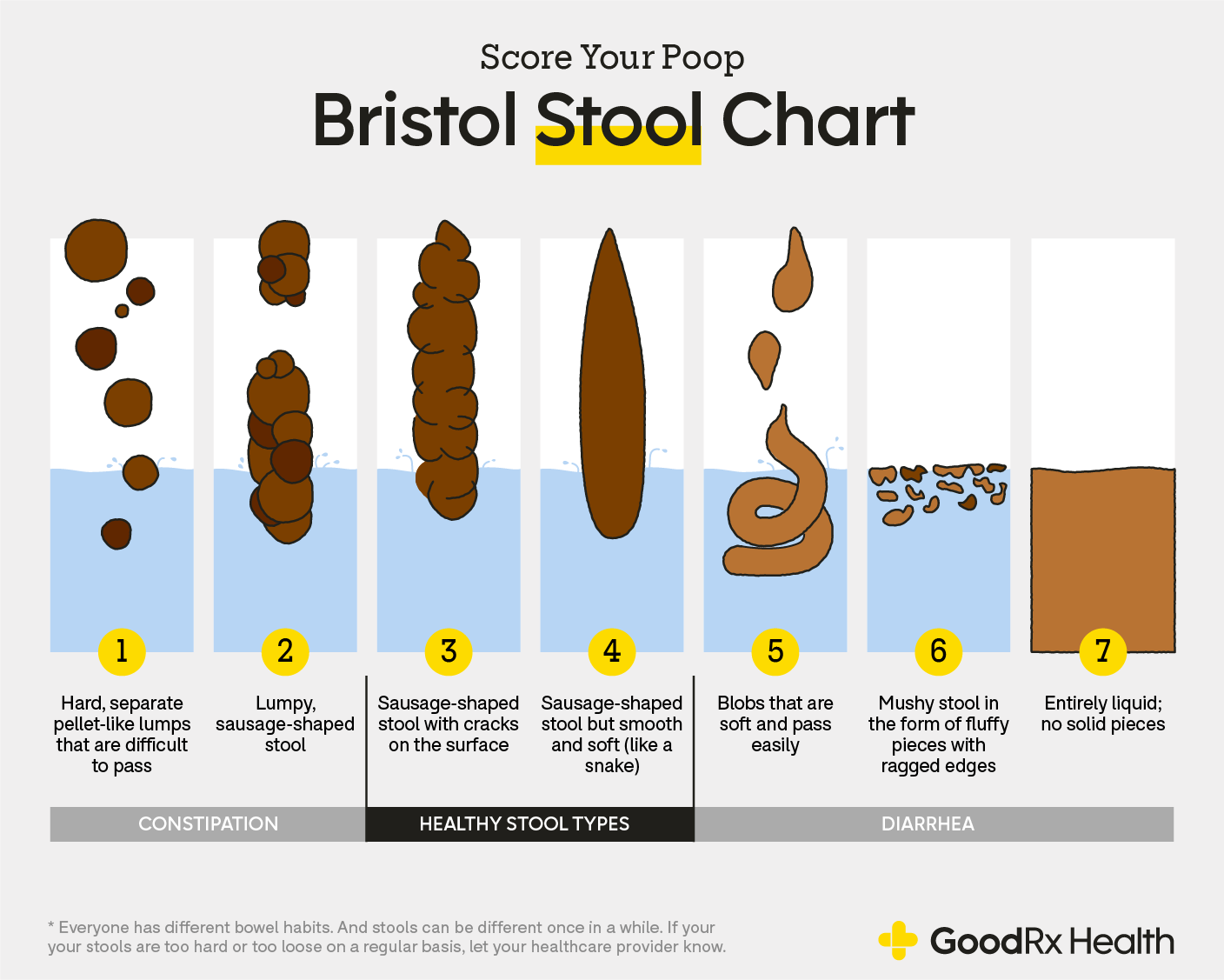
Constipation is defined as:
- Going less than 3x/week
- Difficult passing stool or incomplete bowel movements
- Hard and dry stools (Does the term rabbit poop come to mind?)
- Painful bowel movements
Constipation can be a frustrating and painful condition and can be caused by many different factors including:
- Medical conditions (common ones include hypothyroidism, diabetes, IBS)
- Food allergies and sensitivities
- Poor diet and/or dehydration
- Medication side effects
- Nerve or muscle injuries
- Stress or trauma
- Lack of exercise or mobility
- Post surgical complications
13 Strategies to Beat Constipation from a Pelvic PT
1. Pelvic PT! Constipation can be caused by an overactive or dyssynergic (uncoordinated) pelvic floor. Your pelvic PT can help you figure out if this is part of your problem and also guide you in the following suggestions, telling you which ones would be appropriate for you to try.
2. Drink enough water. Try drinking half of your body weight in ounces of water per day. Example: weight 140 lbs, drink 70 oz of water.
3. Eat enough fiber. You can simply do a google search for “high fiber foods” but the most popular ones include oats, leafy green veggies, dried fruits, beans.
4. Move more. Exercising, especially in the form of a walk after a meal, can kickstart peristalsis in the gut and get things moving.
5. Get more sunshine. Your GI tract is closely linked with your circadian rhythms – You know those people that poop like clockwork every morning at 9am? Getting 5-20 minutes of sunlight into your eyes within 1 hour of waking will help your bowels AND your sleep. Combine this with a morning walk and you have a double whammy!
6. Try a good quality pro- or pre-biotic. Everyone reacts differently to these, start with a cheap one and work your way up if they are not effective. Instead of taking a pill, you can also try eating kefir or drinking low sugar kombucha. (Careful with this if you have been diagnosed with SIBO)
7. Try Psyllium Husk. This is a soluble fiber that absorbs water and sweeps things down the digestive tract. You can eat it straight (start with 1 tsp) or you can mix it in yogurt, oatmeal, baked goods, or smoothies.
8. Eat (or supplement) enough magnesium. Magnesium citrate powder (Natural calm brand, original flavor) at night mixed in tea is a nice way to bump up your intake. Food sources: almonds, chia seeds, spinach, avocados, bananas, oats.
9. Make sure your other micronutrients are in check – these are the vitamins and minerals. Big ones for constipation are magnesium, potassium, B1 (thiamine). You can take a multivitamin or search for foods that meet the RDA for each of these.
10. Try abdominal massage and deep breathing. Tapping into your parasympathetic nervous system helps us to rest and digest. Deep breathing massages the vagus nerve and our intestines, while increasing a sense of relaxation. Massage is a nice way to slow down and give some tactile love to our tummies.
11. Check your stress levels. Stress can wreak havoc on the gut, either in the form of constipation or diarrhea. Talk to your providers about ways to manage stress so that it is less likely to affect your physical health.
12. Do a food journal and track your BMs. Sometimes it’s as simple as one food is stopping you up. Too much cheese? You won’t know until you track your food and your bowel results. Your provider can help you interpret the journal.
13. Visualization and meditation. Visualizing healthy bowels through meditation or affirmations can be the missing link with constipation that hasn’t responded to the other suggestions. Speaking positively about your body and being encouraging can make all the difference. Ask your provider about this and they can help guide you.

This blog was written by Dr Stephanie Hope. Stephanie earned a Bachelors of Science Degree in Psychology from The University of Georgia and then later went on to graduate with her Doctorate of Physical Therapy from The University of North Georgia. She is originally from the southeast, born in South Carolina but raised most of her life in Georgia. Stephanie specializes in pelvic floor dysfunction and this has become her passion within the PT profession. She treats a wide range of women’s and men’s health issues, including incontinence, pelvic pain, and pelvic post-op complications. She is also experienced in treating musculoskeletal and orthopedic conditions and is certified in dry needling.